Shuler had hoped to develop a computer model of a multi-organ system, but there were too many unknowns. The living cell culture system he dreamed up was his bid to fill in the blanks. For a while he played with the concept, but the materials simply weren’t good enough to build what he imagined.
“You can force mice to menstruate, but it’s not really menstruation. You need the human being.”
Linda Griffith, founding professor of biological engineering at MIT and a 2006 recipient of a MacArthur “genius grant”
He wasn’t the only one working on the problem. Linda Griffith, a founding professor of biological engineering at MIT and a 2006 recipient of a MacArthur “genius grant,” designed a crude early version of a liver chip in the late 1990s: a flat silicon chip, just a few hundred micrometers tall, with endothelial cells, oxygen and liquid flowing in and out via pumps, silicone tubing, and a polymer membrane with microscopic holes. She put liver cells from rats on the chip, and those cells organized themselves into three-dimensional tissue. It wasn’t a liver, but it modeled a few of the things a functioning human liver could do. It was a start.
Griffith, who rides a motorcycle for fun and speaks with a soft Southern accent, suffers from endometriosis, an inflammatory condition where cells from the lining of the uterus grow throughout the abdomen. She’s endured decades of nausea, pain, blood loss, and repeated surgeries. She never took medical leaves, instead loading up on Percocet, Advil, and margaritas, keeping a heating pad and couch in her office—a strategy of necessity, as she saw no other choice for a working scientist. Especially a woman.
And as a scientist, Griffith understood that the chronic diseases affecting women tend to be under-researched, underfunded, and poorly treated. She realized that decades of work with animals hadn’t done a damn thing to make life better for women like her. “We’ve got all this data, but most of that data does not lead to treatments for human diseases,” she says. “You can force mice to menstruate, but it’s not really menstruation. You need the human being.”
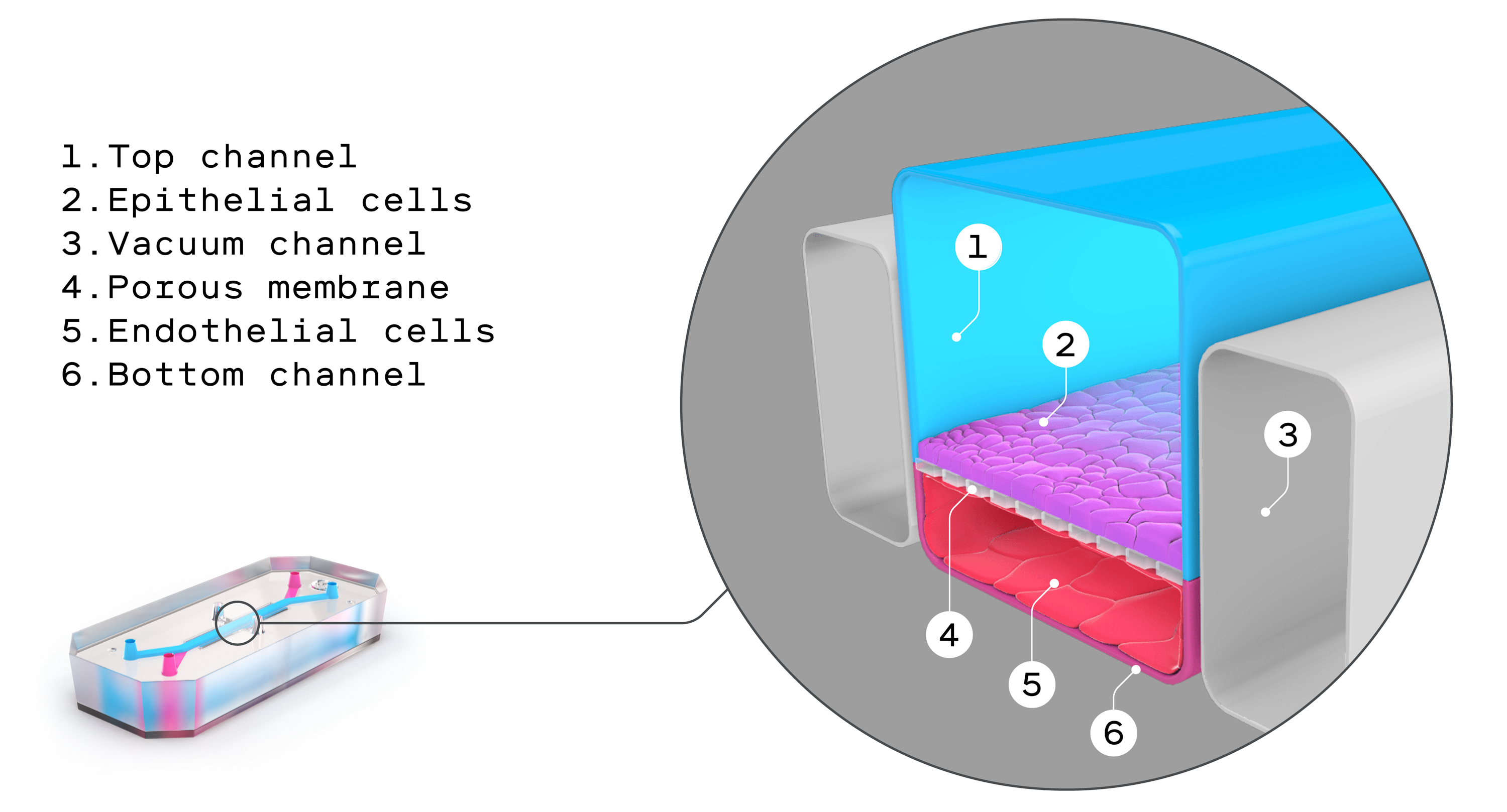
Or, at least, the human cells. Shuler and Griffith, and other scientists in Europe, worked on some of those early chips, but things really kicked off around 2009, when Don Ingber’s lab in Cambridge, Massachusetts, created the first fully functioning organ on a chip. That “lung on a chip” was made from flexible silicone rubber, lined with human lung cells and capillary blood vessel cells that “breathed” like the alveoli—tiny air sacs—in a human lung. A few years later Ingber, an MD-PhD with the tidy good looks of a younger Michael Douglas, founded Emulate, one of the earliest biotech companies making microphysiological systems. Since then he’s become a kind of unofficial ambassador for in vitro technologies in general and organs on chips in particular, giving hundreds of talks, scoring millions in grant money, repping the field with scientists and laypeople. Stephen Colbert once ragged on him after the New York Times quoted him as describing a chip that “walks, talks, and quacks like a human vagina,” a quote Ingber says was taken out of context.
Ingber began his career working on cancer. But he struggled with the required animal research. “I really didn’t want to work with them anymore, because I love animals,” he says. “It was a conscious decision to focus on in vitro models.” He’s not alone; a growing number of young scientists are speaking up about the distress they feel when research protocols cause pain, trauma, injury, and death to lab animals. “I’m a master’s degree student in neuroscience and I think about this constantly. I’ve done such unspeakable, horrible things to mice all in the name of scientific progress, and I feel guilty about this every day,” wrote one anonymous student on Reddit. (Full disclosure: I switched out of a psychology major in college because I didn’t want to cause harm to animals.)
EMULATE
Taking an undergraduate art class led Ingber to an epiphany: mechanical forces are just as important as chemicals and genes in determining the way living creatures work. On a shelf in his office he still displays a model he built in that art class, a simple construction of sticks and fishing line, which helped him realize that cells pull and twist against each other. That realization foreshadowed his current work and helped him design dynamic microfluidic devices that incorporated shear and flow.
Ingber coauthored a 2022 paper that’s sometimes cited as a watershed in the world of organs on chips. Researchers used Emulate’s liver chips to reevaluate 27 drugs that had previously made it through animal testing and had then gone on to kill 242 people and necessitate more than 60 liver transplants. The liver chips correctly flagged problems with 22 of the 27 drugs, an 87% success rate compared with a 0% success rate for animal testing. It was the first time organs on chips had been directly pitted against animal models, and the results got a lot of attention from the pharmaceutical industry. Dan Tagle, director of the Office of Special Initiatives for the National Center for Advancing Translational Sciences (NCATS), estimates that drug failures cost around $2.6 billion globally each year. The earlier in the process failing compounds can be weeded out, the more room there is for other drugs to succeed.

